A breast cancer diagnosis is a rollercoaster ride that no one signs up for. At every twist and turn, the unknowns seem too many to count, the emotional ups and downs never seem to cease and there’s no brake to make the dreaded journey stop. Unfortunately, 1 in 8 women in the United States will face that reality in her lifetime.

Dr. Bing Yu, associate professor in the Joint Department of Biomedical Engineering of Marquette University and Medical College of Wisconsin, is developing an innovative imaging tool that can more accurately and quickly detect tumor margins during breast conserving surgeries. Yu is working with co-investigators Dr. Dong Hye Ye, assistant professor of Computer Science at Georgia State University, Dr. Taly Gilat-Schmidt, former professor of MU-MCW Biomedical Engineering, as well as clinicians Drs. Tina Yen and Julie Jorns from MCW.
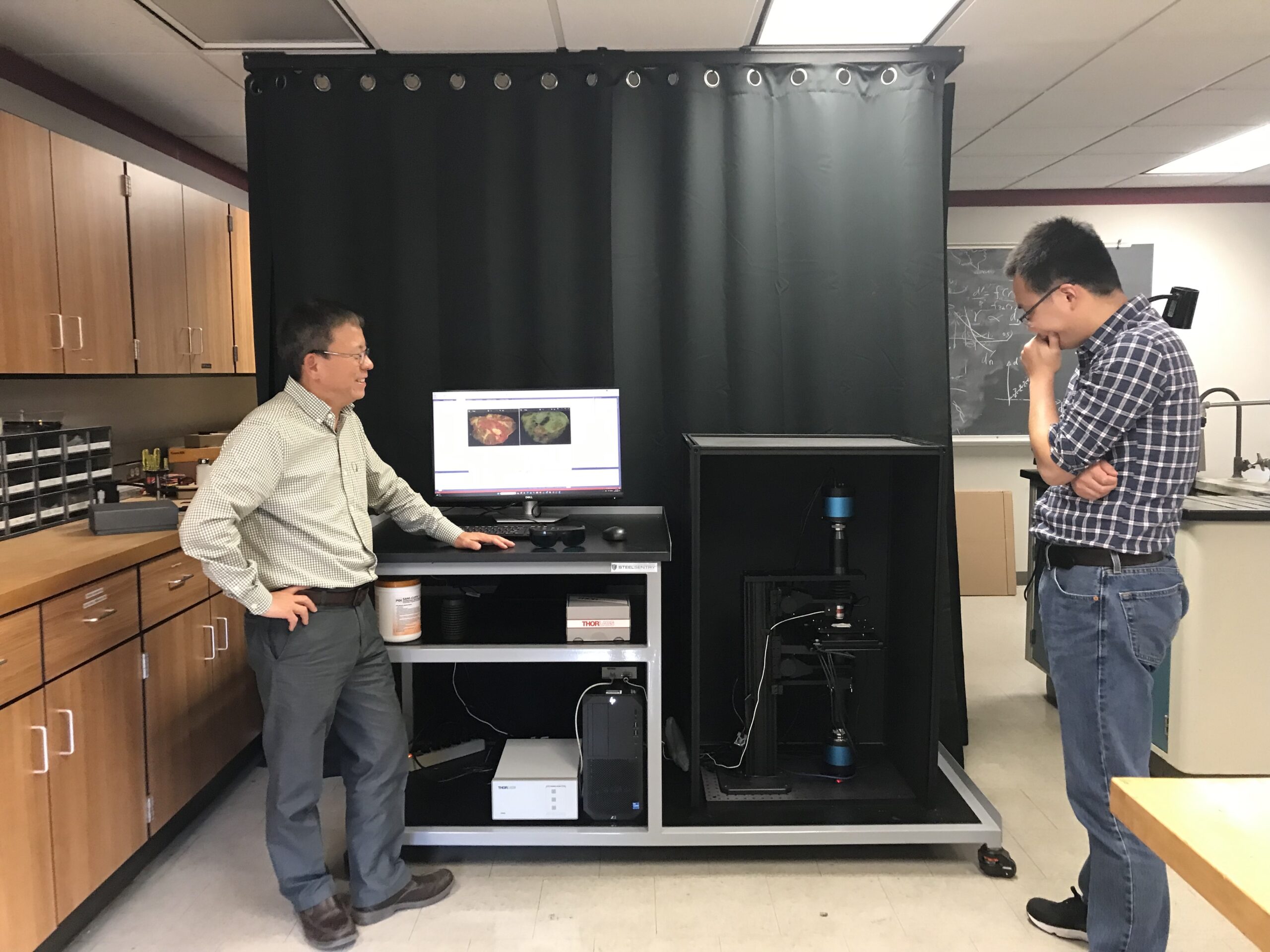
“Our projects are focused on developing an optical microscope that can rapidly survey all surfaces of a freshly resected tumor specimen at high resolution and report if a margin (surface) is clear or if positive cancer cells are found,” Yu says.
He goes on to explain that “if one or more margins are determined to be positive while the patient is still in the operating room, the breast surgeon can go back and shave more tissue from the corresponding location(s) in the tumor cavity until a clear margin is achieved.”
This type of tool will aid in reducing the possibility of leaving cancer cells in the patient after the primary surgery, which could ultimately lead to an additional surgery.
Here in a Q&A, Yu explains how this technology has the potential to decrease the need for a second surgery, as well as emotional stress and costs.
You’re developing more advanced optical imaging and using AI technologies to achieve better breast tumor margin assessments. Can you explain how that’s being done through your research?
Simply speaking, our microscope shines ultraviolet light on the surface of the excised tumor mass that is topically stained with propidium iodide (stains cell nuclei) and eosin Y (stains connective tissue and cytoplasm) and detects the fluorescence emissions. Large specimen surfaces are automatically scanned by the microscope. Our deep learning algorithm analyzes the images during scanning, looking for cancer optical contrasts, such as cell size, cellular density, infiltration, nuclear pleomorphism and nuclear to cytoplasmic ratios, that can be used to differentiate breast cancer cells from normal/benign tissues.
What’s your role in the research process? What are you working on specifically to make these medical advances happen?
I am leading a large multidisciplinary team, including biophotonics and computer engineers, a breast surgeon, a breast pathologist, MCW Tissue Bank staff, a clinical research coordinator, a postdoc and graduate students. We are currently developing our second-generation microscope hardware, software and AI algorithms and testing the device on surgical tissues from the MCW Tissue Bank.
How will this research benefit individuals with a breast cancer diagnosis? Is this technology a game changer in the medical field?
The project is significant because it addresses the unwanted scenario of needing to perform additional surgery for over 20,000 women annually in the U.S. after breast conserving surgery due to positive margins. During surgery, if the device identifies positive margins, surgeons will remove additional tissue at the site(s) of positivity while the patient is still in the operating room. Successful development of the technology will reduce re-excision rates for hospitals and facilities where the rate of positive margins is high and where current margin assessment techniques are not routinely available or utilized. Decreasing rates of positive margins will reduce the need for additional surgeries thereby improving oncologic outcomes (delays in adjuvant treatment, local recurrence rates), patient satisfaction (anxiety, cosmesis) and economic burden (costs of additional surgeries and income loss due to recovery from surgeries) to patients, their caregivers and health care systems.
Do you see this type of technology crossing over to detecting other types of cancer in the future?
Yes, we are developing a platform technology that can be easily adapted for many other types of cancers, like head and neck, prostate, pancreatic cancers, etc.
How does it make you feel knowing that your research is helping save lives?
I would love to see that our technology is used in the clinic to help both the physicians and patients. That would be a big accomplishment.
When do you see these advancements being used in the future by doctors and medical professionals? Is it in the near future?
Due to the translational nature of the study, we expect that the device will be available for use in the operating rooms within five to 10 years.