Nursing is generally regarded as a science. Nursing courses are all in the sciences. Anatomy, physiology — all deeply scientific. It even reads “Bachelor of Science” or “Master of Science” on nursing diplomas.
However, to College of Nursing faculty member Dr. Jay Tumulak, nursing is equal parts science and art.
“In the beginning, nurses stick to the prescription,” Tumulak says. “In a particular patient, given a particular weight, you give a particular dose. As you practice, though, you begin to realize that different ages and different patients have different physiological functions. You trust your intuition more.”
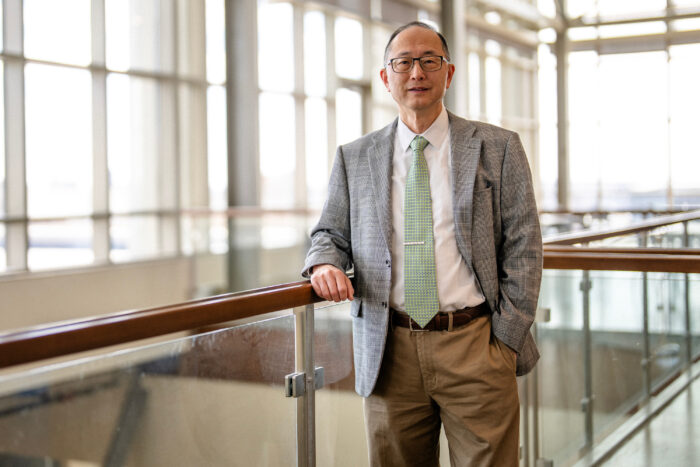
Tumulak, a clinical assistant professor and the Associate Director of the college’s Nurse Anesthesia Educational Program, has had a long time to hone that intuition after more than 30 years as a practicing nurse and almost 15 as a professor. The American Association of Nurse Anesthesiology recognized his accomplishments recently by inducting him as a fellow, an honor that distinguishes a clinician as one of the profession’s most well-credentialed leaders.
“We are not measured by how well we adhered to exactly how much drug our textbook says to give; we are measured by our outcomes.”
Dr. Jay Tumulak, Associate Director of the Nurse Anesthesia Educational Program
The email notifying Tumulak of the honor came in April, telling him he would receive a formal induction in front of his peers at AANA’s annual conference. He immediately called his wife, overjoyed with the good news.
“I owe her a lot; her patience and support have really been instrumental,” Tumulak says. “I never really thought I would get to do that. The years I spent working as an academic and a clinician paid off.”
Those years started in Tumulak’s native Philippines, on the tropical island of Cebu. Tumulak initially wanted to become a doctor, but nursing gave him a clearer path to the United States, where he had hoped to start a career. His interest in advanced practice steered him to nurse anesthesia.
“Anesthesia is very fast-paced, and you have to be able to function independently with very acute critical thinking,” Tumulak says.
When Tumulak joined Marquette in 2018, the nurse anesthesiology program — the first in Milwaukee — had just admitted its first cohort.
“Before we establish a program, we always have to verify that there’s a need for it,” Tumulak says. “Based on research, we found that there were not enough clinicians providing these services in Milwaukee. It was the right time and the right place to establish the program.”
“One of the greatest services our college can provide the profession is to play our part in addressing the nursing shortage,” says Dr. Jill Guttormson, dean of Marquette’s College of Nursing. “This program helps us progress toward that objective by meeting the need for highly trained, compassionate nurse anesthetists.”
Students in the program, which is administered by Tumulak and Clinical Associate Professor Dr. Lisa Thiemann, are already experienced nurses and usually have a CCRN certification, an advanced professional designation that signifies specialization in providing care to critically ill patients. Faculty interview prospective students to ensure they are the right fit to become a nurse anesthesiologist and can withstand the program’s rigor.
Matt Brune, a second-year nurse anesthesiology student, came back to Marquette after graduating with an undergraduate nursing degree in 2016 and practicing alongside nurse anesthetists in acute care settings. He says much of the program’s impact is attributable to its leadership.
“This program is great because of the direction that Jay and Lisa provide,” Brune says. “They pay outstanding attention to the quality of the education we get and the kinds of people we train with. They’re also very responsive to what can facilitate the learning process best for us as students.”
Clinical experience is of paramount importance for Tumulak, who still practices at a hospital in Illinois and is also a member of the state’s nurse anesthesiology association. He sees it as the best way to keep his teaching current and give students the best possible representation of what their careers will be like.
“While I am able to teach the students science in the classroom, nurse anesthesia as an art gets developed in the clinical settings,” Tumulak says. “The students appreciate when you can tell them, ‘This is what happens in a hospital and I’m giving you this example or that one from the patient I took care of a couple of days ago.’”
Research is also important to Tumulak. In 2017, he spearheaded a study into a new method of relieving spinal surgery pain using a capsule loaded with a local anesthetic. The anesthetic would deliver sustained relief without the addictive qualities of opioids, such as morphine. He continues to be cognizant of the innovative approaches to ensure the best patient outcomes.
The study, Tumulak says, is a microcosm of a nurse anesthesiologists’ true calling: to ensure patient comfort and safety. Surgical patients rely on professionals like Tumulak and his students to get them through one of the most difficult experiences they will ever have.
“We are not measured by how well we adhered to exactly how much drug our textbook says to give; we are measured by our outcomes,” Tumulak says. “That’s where the art of it comes in; how can we balance patient safety with a plan of care that’s more personalized?”
It is never an easy tightrope to walk, but successfully doing so for decades has earned Tumulak a place among his profession’s absolute best.