More than three million babies are born every year in America. Certified Nurse-Midwives are an important group of health professionals who can meet the needs of pregnant people and their families. Most CNMs provide care in hospitals, but some work in birth centers and assist with home births.
“We are trying to make nurse midwifery the standard practice of care for low-risk individuals, like it is in other countries,” says Dr. Kathlyn Albert, clinical assistant professor and the director of Marquette’s Nurse-Midwifery Program.
The College of Nursing houses the only accredited nurse-midwifery program in Wisconsin and one of just 44 such programs nationally. For three decades, students have come to Marquette for a master’s or post-master’s level offering that prepares them to help individuals at every stage of the birthing process. Many in the nurse midwifery profession say it’s more than a career — it is a mission. Nurse-midwifery care extends beyond childbearing and includes primary and gynecologic health care for women from menarche through post menopause.
“It was a spiritual calling for me; it feels like what I was meant to do,” says Dr. Lisa Hanson, the program’s associate director.
Before coming to Marquette, Hanson practiced as a nurse in Milwaukee, where she witnessed births that were not woman centered. She knew early on she was drawn to make woman centered birth her life’s mission.
“I was seeing what I viewed as insensitive treatment of healthy women during labor and birth,” Hanson says. “Women were being directed at to push even when they had no desire to do so; often they would be flat on their backs. Many of them weren’t being asked what they wanted to do; rather they were being told what to do. I thought to myself, ‘There has to be a better way.’”
Finding a better way for patients is a nurse-midwife’s goal. Graduates from the NMP are entrusted caring for individuals from adolescence through older adulthood, including pregnancy through the postpartum period, as well as the ability to offer primary care and gynecologic services.
Nurse-midwives are educated to recognize the parameters of normalcy in pregnancy and areas aspect of health care and make shared decisions with patients to achieve a safe and satisfying outcome. Collaboration with other health care professionals including physicians is essential to midwifery practice. Therefore, patients who develop complications can be safely cared for by CNMs using consultation, referral and/or transfer of care, as appropriate.
“We like to think about it as us being a team with our patient,” says Alexis Manley, an NMP student. “Instead of it being a hierarchy where a doctor tells you what you need to do and how you need to do it, we’re having conversations about what our patients want and what our current research shows.”
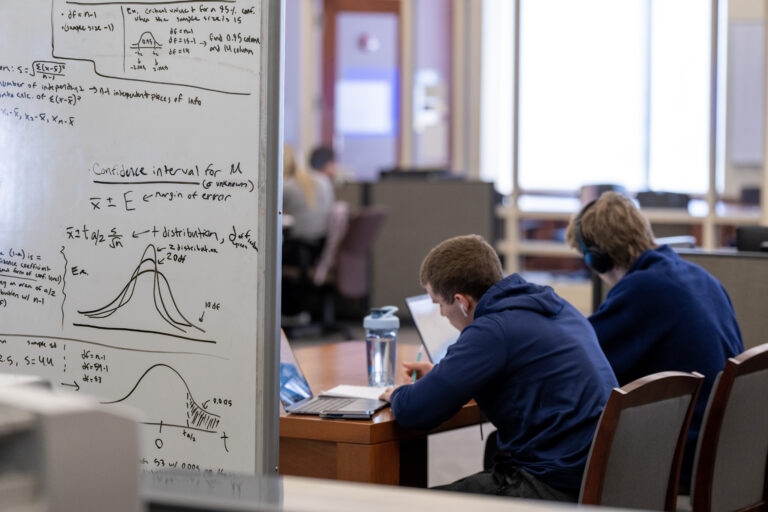
Students in the NMP take a 49- to 51-credit, hybrid-online format series of classes. Theory is largely done either synchronously or asynchronously online, while simulations and clinical learning is conducted in-person. The program also guarantees students clinical placement through its partners throughout Wisconsin and northern Illinois, supplementing their in-class learning with precepted clinical experiences.
Among the already limited number of midwifery programs in the country, even fewer can assure clinical placements for students. Manley participates in precepted clinical learning with the midwifery practice at Meriter Hospital in Madison, scheduling clinicals around her class schedule.
Originally a psychologist, Manley changed her path after working alongside labor and delivery nurses at a small community hospital in Elkorn, Wisconsin. Her time at Meriter with her midwifery preceptors has reinforced her commitment to the nurse-midwifery profession.
“They are super welcoming and want to teach me,” she says. “Having the access to them without the stress of searching for them myself was a big benefit of the program. Marquette has the resources and the relationships with health care systems to make this easy on students, which is great.”
NMP uses a cohort model; students come into the program in groups of up to 10 and stay with the same peers until graduation. It’s a similar format to the college’s Nurse Anesthesia Educational Program. Allowing students to work closely with student colleagues over a longer period promotes camaraderie and trust, fostering learning and social support. It also gives the graduate midwifery students a community of belonging.
Cherise Edwards entered the program in 2021 and is expected to graduate in May. Although Edwards already received an undergraduate nursing degree, she felt that Marquette’s combination of rigor and personal attention was the right mix to move her career forward.
“It has been super easy to get into this new routine of being a midwife and doing what I’m so passionate about; it’s been a real blessing,” Edwards says.
Marquette Nursing teaches the profession through the lens of the college’s core values; the introductory-level undergraduate nursing course is even called “Nursing and Health in the Jesuit Tradition.” During that course and others, Marquette Nurses are taught to apply the concept of cura personalis — caring for the whole person — to their patients, seeing the context of their lives instead of just a collection of symptoms. That line of thinking is a natural fit for the NMP.
“Nurse midwives look at patients holistically and that’s why it’s such a great fit with Marquette,” Albert says. “Being a primary care provider, we tend to spend quite a bit of time with our patients and get to know them. We’ll often see them through primary care situations first and then, when they become pregnant, we’ll continue that nurse-midwifery model of care. We are also trained to care for newborns up until 28 days of life.”
Most babies in the world are born into the hands of midwives. In the U.S., midwives attended just 12 percent of the country’s births. Countries such as Australia, Sweden, Norway and the United Kingdom all had over 10 times as many midwives per 1,000 live births as the U.S. did as recently as 2018.
Hanson and Albert hope to change this reality. They dream of a time when there will be enough CNMs to meet the needs of pregnant people and their families.
“It takes a lot of dedication because the life of a midwife involves irregular sleep, irregular eating and sometimes missing time with your family,” Hanson says. “It takes a special person who’s willing to adjust that balance in their lives on behalf of other people.”
Albert adds, “The number one most rewarding thing for a CNM is to develop a bond with patients and then be there for one of the biggest events of their lives.”