When the COVID-19 pandemic came to America in March 2020, it impacted daily life for everyone, as public gathering spaces closed and people quarantined in their homes.
However, the severity of its impact was not equitable.
The pandemic fell especially hard on groups who did not have the same defenses against COVID as their peers. Elderly patients were one of the most imperiled groups; according to the Centers for Disease Control, 81% of COVID deaths in 2020 were among people age 65 and older.
That reality placed another group of people in the center of the storm: acute care gerontology nurses.
“Our students are the ones who were providing care in the hospital to the most vulnerable COVID patients and being immersed in that bedside practice,” said Felisa Antonchorgy, clinical adjunct faculty member in the College of Nursing’s Adult-Gerontology Acute Care Nurse Practitioner program. “It put us in a position where we had to re-examine our priorities to ensure that while we were still maintaining excellence while also taking care of students.”
COVID-19 marked a new era for the AGACNP, one in which trends that applied to the nursing profession were exacerbated among those delivering elder care. Burnout rates were higher. The proportion of nurses who worked on overloaded hospital floors was greater. Staffing issues were even more dire.
With those 65 years and older set to account for 22% of the country’s total population by the year 2040, America can ill afford to be short on qualified nurses.
“The population is aging and the average patient in hospitals is getting older, so we need to be aware of their needs and specialties,” says Dr. Debra Casper, program director of the AGACNP and a clinical instructor. “The other piece of this is a shortage of beds and facilities. Not only is there a nursing shortage for positions, there’s a shortage in all areas of elder care. The role of AGACNP is for Marquette to fill a gap for providers.”
Casper, who began teaching at Marquette in 2008, came with a background in trauma and critical care. When she first arrived in Clark Hall, Marquette was the only college in the Milwaukee area to have an acute care nurse practitioner program; it added a focus on adult and gerontological care in 2012. That has changed within the past few years; the University of Wisconsin–Milwaukee and Alverno College have started AGACNP programs. As COVID shifted from pandemic to endemic, the higher education community recognized how essential it would be to keep the profession’s ranks strong.
“These last few years have created a profession that’s more willing to use its collective voice.”
Felisa Antonchorgy, clinical adjunct faculty member
“Lots of people across the state and across the nation were contacting us and asking how we were managing our program during COVID,” Casper says. “That’s the power of Marquette networking: we were able to provide for students, but we were also able to provide resources to our preceptors in hospitals because of the expertise we have here. Both are essential for making sure acute gerontology nurses get into the business and stay in it long-term.”
Marquette offers three distinct options for its AGACNP: a post-master’s certificate, a Master of Science in Nursing and a Doctor of Nursing Practice. The program contains about 80 students, with approximately 18 to 24 per graduating class. Learning takes place in a mix of in-person and online formats, with guaranteed clinical placements giving students exposure to what life after graduation would be like.
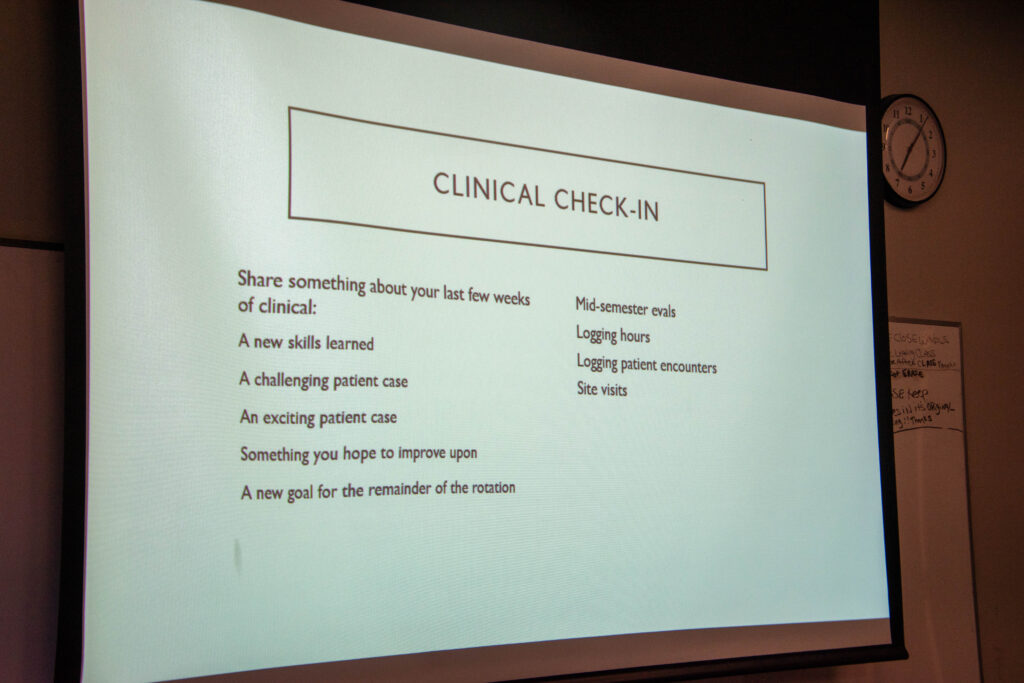
Since COVID, Antonchorgy and Casper have made mental well-being more of a priority in the course as a response to the strain the pandemic put on gerontology nurses.
“Every day, I start my class with my students by asking them how they’re doing and what’s going on in their lives, and I never started it that way in pre-pandemic times,” Casper says.
“I think we’re all more aware now of the self-care needs and how that needs to be a focus both in education and in life,” Antonchorgy says. “Maybe in the past, we would have reacted to a late assignment by telling students to manage their time better and asking why they couldn’t have gotten it done. Now we’re a lot more sensitive to what else students have going on in their lives.”
One of the other changes Casper made to the program is the MSN graduating cohort community service project, an initiative that started during the 2022-23 academic year with a clothing drive for Milwaukee-area hospital patients. Each class of graduating AGACNP seniors plans and executes a project that addresses health care inequity, in alignment with the core Marquette Nurse quality of advocating for the vulnerable.
Casper wants her students to engage with health care issues outside the hospital more readily.
“As advanced practice nurses, we are looked at as leaders, not just within our own health care organizations but in the community,” Casper says. “For them to live up to that leadership role across the board, we need them to engage in activities outside going to the hospital and doing their schoolwork. They need to recognize the impact they can have on society has a whole.”
After a slight decrease during COVID, admissions to the program have rebounded and are back to historical averages. These new graduates will be even better equipped to care for themselves and others and will not be shy to speak up about the systemic problems the pandemic revealed.
“These last few years have created a profession that’s more willing to use its collective voice,” says Antonchorgy.



