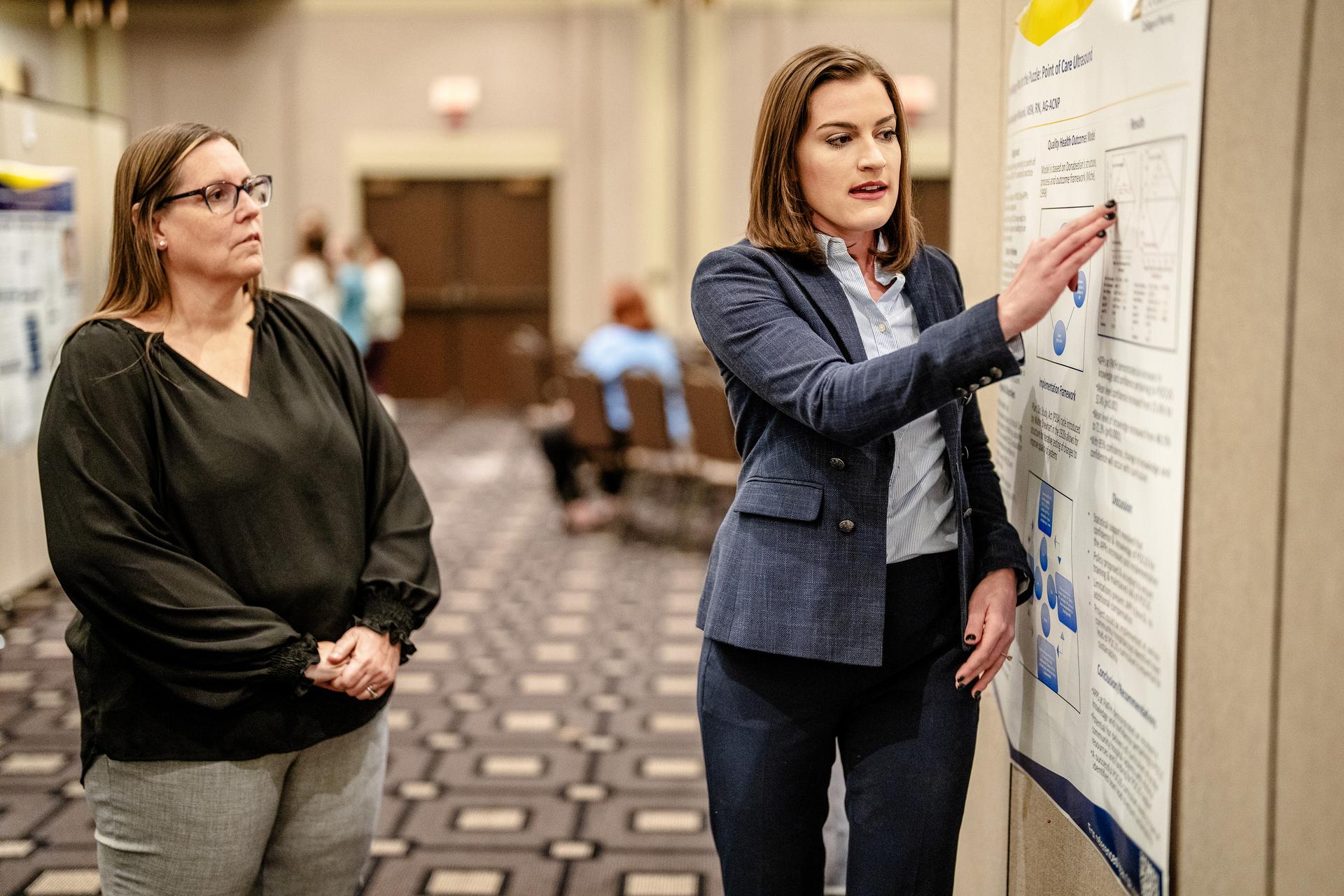
Dr. Jillene Saler, a Class of 2024 graduate of Marquette’s Doctor of Nursing Practice program, spent months figuring out how to improve patient outcomes through her DNP practice change project.
“This project is all about looking at something you can make better, whether that’s an educational, process or support issue,” Saler says. “Before I became a nurse practitioner, I worked in the ICU. I knew I wanted to do something in that realm to improve outcomes and help people I’d worked with for a very long time.”
Diverse professional and personal backgrounds, not to mention a shared commitment for continuous evidence-based improvement, make up the bedrock of effective practice change projects. After completing quality improvement, informatics, epidemiology, and several other important doctoral-level courses, students create a proposal to identify and generate solutions to a problem in their own health care organizations, work with key personnel to implement them and systematically evaluate the results. Project completion is required for graduation from the DNP program.
It’s a little bit addictive. Once you start improving things, you want to fix the next thing.
Dr. Kathleen Summers, Class of 2023 DNP graduate
The practice change project is one of the main differences between a DNP and Ph.D. education. Although both are doctoral-level degrees, the Ph.D. candidate is more focused on creating new knowledge and conducting research. While there is a research component to a DNP curriculum, doctors of nursing practice use evidence from that research to inform their clinical practice.
“The nurse who holds a DNP is prepared to be a systems thinker and leader,” says Dr. Sandi Kaebisch, director of Marquette’s DNP program. “The DNP in the clinic, hospital or community approaches process or systems issues from a 360-degree perspective, leading teams and providing their expertise and using evidence to identify and solve problems.”
DNP students at Marquette have a long history of meaningful contribution to their health care systems through practice change projects. Initiatives to fund vision exams in schools serving at-risk children, encourage adaptation of opioid-free anesthesia and improve antibiotic usage among pediatric urgent care patients are some of the sustainable practice changes created by Marquette DNP graduates.
“It’s a little bit addictive,” says Dr. Kathleen Summers, a Class of 2023 DNP graduate. “Once you start improving things, you want to fix the next thing.”
The road to seeing improvement can be a long one, however. Saler spent four months reading the research, crafting her proposal, preparing educational interventions for hospital staff, and attending numerous staff meetings to get buy-in. After approval, she led the six-week intervention, continuously improving the process in real-time. Following months of data collection and evaluation, Saler shared her findings with the hospital staff and the community at the DNP Symposium at Marquette. While Saler’s practice change project was successful and is still used today by her health care system, she contends that it took more than just a good idea: execution was crucial.
“You have to rely on your stakeholders and keep lines of communication open; using your clinical nurse specialists and the managers on your unit will help things go a lot more smoothly,” Saler says.

While some practice change projects address procedural issues, others address educational questions. Dr. Tracy Blair, a DNP graduate and Marquette clinical instructor, noticed that her clinical students would often not know where to go for the most reputable information on practice-related questions. She then noticed that some of her coworkers had similar issues, which prompted her to pursue a project titled “Impact of Education on Critical Online Reasoning.” Blair used a media literacy educational module that originated at Stanford University as a model to create an educational intervention for nurses specific to the needs of her hospital.
After institutional review board approval, participants in her classes volunteered to have their in-class search histories downloaded by the IT department. Blair analyzed those searches to identify the nurses’ ability to correctly identify reputable sources of information, with the hope that they used more reputable sites after they’d taken the educational module.
“We don’t really teach nurses how to properly look things up on the internet in a systematized way,” Blair says. “I boiled it down to three questions that nurses should keep in mind: Who’s behind the information? What is the evidence? And what do other sources say? This is applicable at any level of nursing.”
The results from Blair’s project were promising enough that it’s been incorporated into new nurse training at her workplace. “Every nurse needs to know how to find good, evidence-based information to care for their patients, and I’m happy that this has become a standard part of their professional development,” Blair says.
DNP graduates often ascend to leadership positions in their organizations—these are jobs that require skills beyond the bedside. Pursuing grant funding, calculating return on investment, applying research to practice and navigating organizational dynamics are all functions that a DNP might have to perform. The practice change project gives students an opportunity to synthesize those skills to make a tangible impact. It’s an experience they carry with them long after they turn in their final assignment.
“These projects are very rewarding because you get to see all of your hard work lead to an actual change in the way things are done in health care,” Saler says.