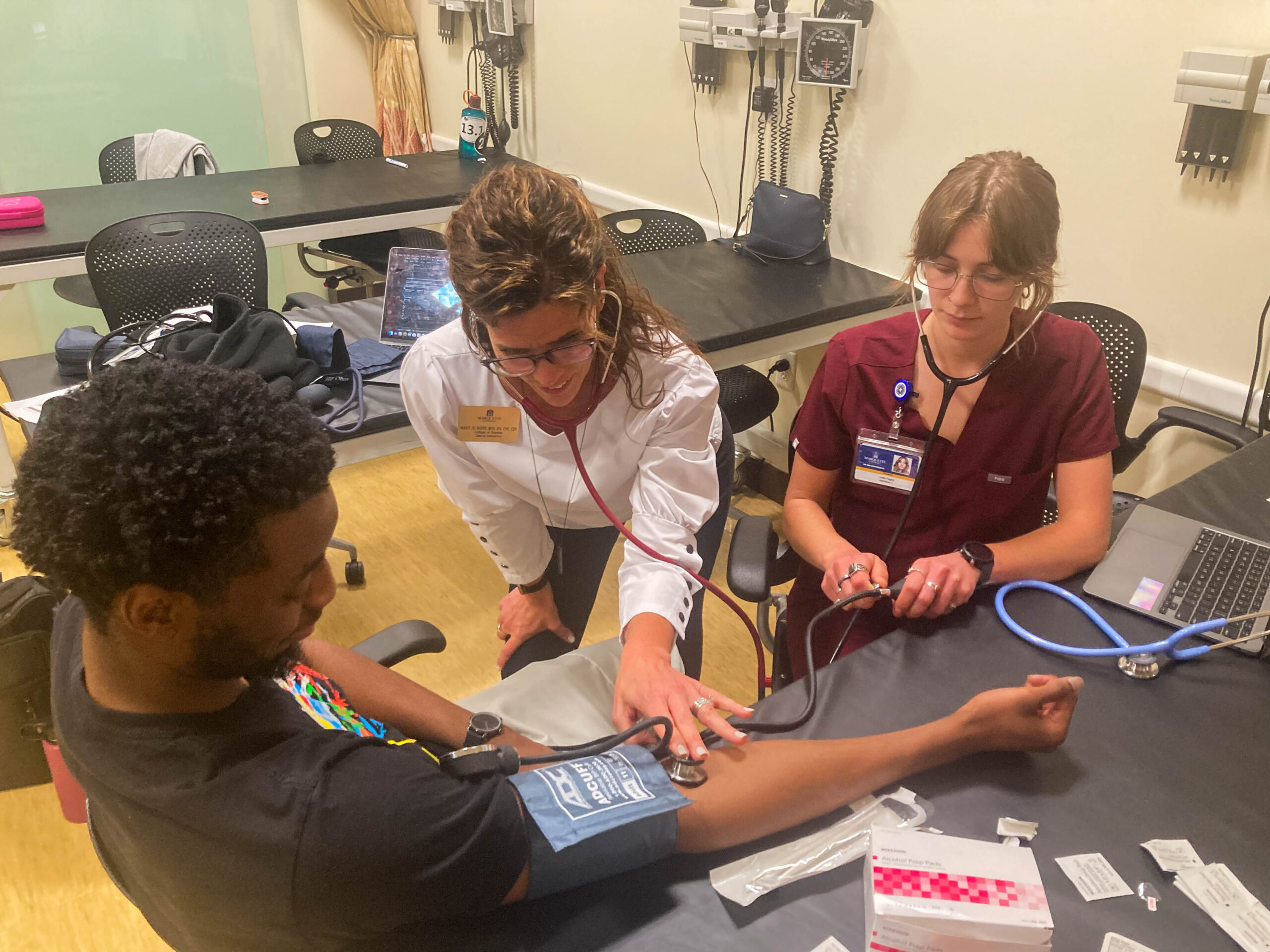
Kiley Huckstorf squeezes the bulb of a blood pressure cuff, which is wrapped around a dental student’s upper arm. She listens carefully for the repetitive tapping of her subject’s pulse, which indicates the systolic blood pressure. Suddenly, she finds it. The tap is faint at first, then it grows more distinct, taking on the sound of swishing as the cuff tightens. It resounds through the stethoscope’s earpiece — lub-dub, lub-dub, lub-dub — growing more muffled until-
Pssstttt….
The noise disappears. The cuff deflates. Clinical Instructor Ashley Ryan, having observed the whole exercise, nods in approval before continuing to the next pair.
“It can be hard to hear what you need to hear when you have a noisy environment, plus a lot of people don’t know what they’re listening for the first time they do it,” Ryan says.
Ryan, who works in the College of Nursing, and Dr. Yasser Khaled, clinical assistant professor in the School of Dentistry, wanted to make this sometimes-challenging process easier on their students by allowing them to practice on each other. The two faculty members brought their classes together for an interprofessional education class, the first of its kind for the Direct Entry Master of Nursing program and a new initiative for first-year students in the School of Dentistry.
“We figured that checking the vital signs for a patient is a necessary basic skill that is essential for both the nursing and the dental students, and we also wanted to teach the nursing students how to do oral examinations.” Khaled says.
This is the second sanctioned IPE activity in the School of Dentistry; the college also recently hosted one for students at Medical College of Wisconsin. Marquette hosts a standing IPE committee that consists of representatives from all health professions to coordinate interprofessional research activities.
The success of those earlier IPE efforts convinced faculty in both colleges to form this new collaboration. Huckstorf found it valuable.

“It was great for us to learn from each other because we both have different experiences,” Huckstorf says. “It’s a learning process. Things were difficult at the start of the session, but we helped each other and it gradually got easier.”
Students of both disciplines attended a joint presentation, touching on proper intra-oral assessment technique and the correct way to feel for a patients’ pulse. Learners then split off into pairs and practiced what they learned on their partners.
“I thought it was a unique experience,” said first-year dental student Mahdi Jaber. “I felt they gave us really good feedback on what to look for when searching for blood pressure and pulse. The nursing students have that experience, whereas we have more experience with the oral cavity and it was nice that I was able to share the information with them.”
While most people assume checking pulses is a baseline skill for nurses, they may not know it’s also vital for dentists. If a patient’s systolic blood pressure is over 180, dentists should not treat that patient due to the likelihood of medical complications, particularly if anesthetics are used. A dentist knowing how to measure heartbeat frequency might be the difference between life and death for some patients.
It’s one thing to like the idea of interprofessional education; it’s another matter to put it into practice. Oftentimes, dental students were taught these skills in groups of close to 100 with just a few faculty in attendance, which necessitated a style of class geared toward a large group. Multiple interdisciplinary sessions over the summer with smaller class sizes allowed students to get more practice, but it required changes in how the class was taught to better fit a different format.
Ryan says flexibility is key.
“It takes a lot of work and communication, but if both parties are willing, it goes well,” she says. “Dr. Khaled and I went back and forth a lot about how we teach and how we see our skills fitting together, and that’s why this was a success.”
The students were just as willing as their instructors, as nurses and dentists exchanged tips for treating patients. Jaber says he learned from his nursing peers that it’s important to look at the stomach more than the chest when assessing a man’s respiratory rate, since men use their abdominal cavity in breathing more than the chest. Wisdom like this will make him a more capable, well-rounded dentist.
“We’re all in the medical field, and there are people that understand different things than you outside the dental clinic and the dental school, and the same goes for them in their areas of study,” Jaber says.
Based on the positive feedback, Khaled says he is confident there will be more opportunities for IPE learning in the future. Collaboration between colleges could very well hold the key to shaping better health care practitioners across professions.