Dr. Kristi Streeter explores the mysterious interaction through which signals from the diaphragm may help rewire the brain to help those with spinal cord injuries breathe better.
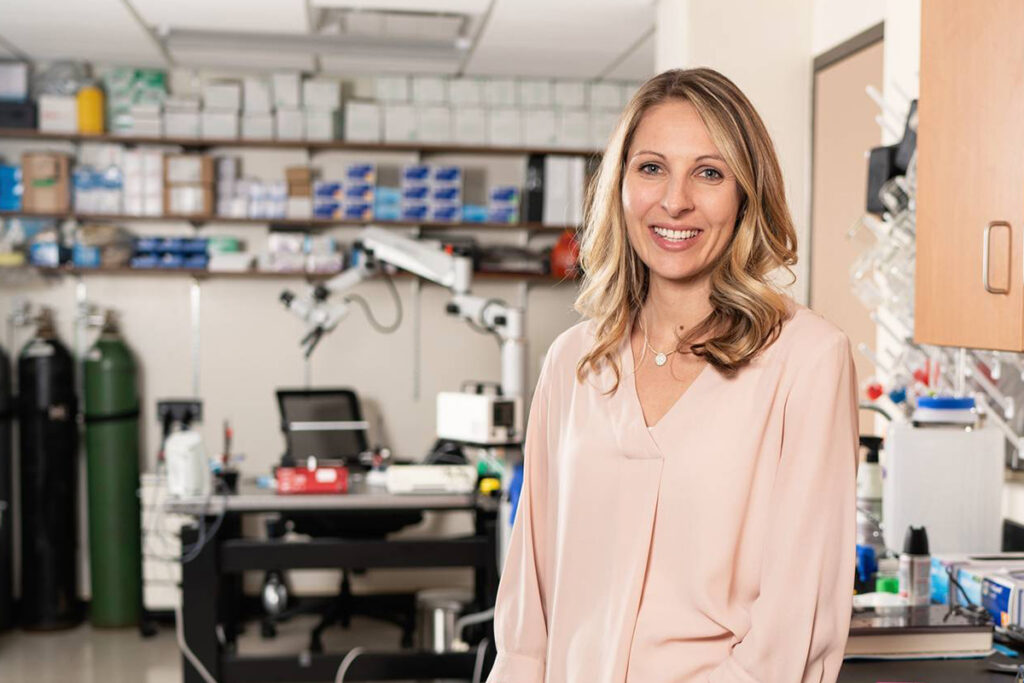
By Carrie Arnold, photo by Kat Schleicher
Every day, we inhale and exhale approximately 22,000 times. Over a lifetime, the breaths we take number in the hundreds of millions. Although we can consciously control our breathing, most of the time we respire without deliberate thought. Even depriving our brains and bodies of oxygen for just a minute or two can be life-threatening.
It’s why improving respiratory function in people with spinal cord injuries is so important, says Dr. Kristi Streeter, assistant professor of physical therapy. In people with the most severe types of neck injuries (affecting the cervical spinal cord that stretches from the base of the skull to the upper back), the neurons that connect the brain to the diaphragm muscle are severed, leaving a person in need of a ventilator to breathe. For those with less severe injuries, however, those nerves remain partially intact. Although many of these patients need help breathing and remain at high risk for respiratory problems like pneumonia, the persistence of some neural connections opens the door for rarely studied healing processes involving neural plasticity to help improve breathing.
That’s where Streeter comes in. She has received a highly competitive $747,000 K99/R00 grant from the National Institutes of Health — a first for Marquette’s Physical Therapy Department — to study neural plasticity involving the neurons that control breathing in people with spinal cord injuries. Like Blackmore, Streeter is advancing science and solutions on the cutting edge of spinal cord injury research, only in her case within the pathway where signals travel from the brain to the spinal cord and down to the diaphragm — and take the reverse course too.
By understanding how this interplay of diaphragm, nerves and brain responds to trauma that leaves the spinal cord partially intact — and how this system can adapt in healing ways — Streeter hopes to help those with neurologic injuries lead better, more fulfilling lives. “We’re really at the tip of the iceberg in terms of what we understand,” she says.

Remembering to Breathe
The impetus to inhale originates deep in the brainstem, in one of the most primitive parts of our nervous system. In humans, as in all mammals, that signal races down the brainstem and into the spinal cord, until it hits the phrenic nerve. Emerging from three spinal cord nerve roots, the phrenic nerve connects the spinal cord and the muscular diaphragm, which bends and flattens as it contracts. When this happens, our lungs can expand and fill with oxygen as we inhale. As the diaphragm relaxes, it forces air out of the lungs. If the spinal cord is damaged above the C5 vertebra, the neural superhighway connecting the brainstem to the diaphragm is damaged. If the spinal cord is severed completely, signals can’t travel to the phrenic nerve and the diaphragm. But if the spinal cord remains partially intact, some connectivity remains, a condition that Streeter can re-create in the lab using rodent models. “The breathing pattern is very similar to what we see in patients,” Streeter says.
The rats respond to this injury by shifting their standard slow and deep breaths to rapid panting. The severed connection, Streeter explains, means that their diaphragm muscles aren’t getting the normal signals to contract. As a result, the lungs can’t fill with oxygen or expel carbon dioxide as well. To compensate for their inability to breathe deeply, the rats take quick, shallow breaths. Humans with similar injuries do the same thing, Streeter says.
Although these patients can still technically breathe, many still require a ventilator to ensure they receive enough oxygen and exhale enough carbon dioxide. But life on a ventilator is risky — and hard. To help some of their patients get off a ventilator, doctors began turning to diaphragm pacing. Similar to a cardiac pacemaker, the diaphragm pacer uses surgically implanted electrodes to stimulate muscle contraction. To the doctors’ and patients’ surprise, the diaphragm pacer enabled some patients to come off a ventilator and breathe on their own.
Then things took a very unexpected turn. Not only were patients able to stop using a ventilator, but over time, many also stopped needing the pacer altogether. “It’s almost as if the pacer activated respiratory memories,” Streeter says. She wanted to know how.
As a doctoral student at the University of Florida, Streeter learned not only how the brain sent messages to the diaphragm muscle to stimulate breathing, but also how the muscle sent messages back to the brain. This latter direction of travel (muscle to spinal cord to brain) is called an afferent. The use of the diaphragm pacer also stimulated these phrenic afferents, and Streeter hypothesizes that it’s the bolstering of this pathway through a process of neural plasticity that helps those with spinal injuries breathe more easily.
“Does the diaphragm paralysis improve if we stimulate these afferents for a while?” she asks. “I want to know the cellular mechanisms that enable this process.” Her new grant will allow her to uncover details about how respiratory neurons receive electrical signals from the diaphragm muscle, and whether artificial electrical stimulation of these neurons will help restore sensory input to the spinal cord. Streeter hopes this neuroplasticity means patients can breathe better.
For Streeter, everything comes back to the patients in the clinic. “I want to know what patients care about, and then go back to the lab and find the way to get there,” Streeter says.
Read the other two parts in this series focusing on Dr. Murray Blackmore’s lab here and the Neuro Recovery Clinic here.